Abstract
It has been recognized and written about the need to integrate skills, knowledge, and hospitality processes into the very complex area of delivering health services to patients/customers over the last couple of years. This has only become even more exasperated with the onset of COVID-19 and the many variants. As we sit here today, according to a variety of statistics including life longevity, we are in an even less desirable situation concerning the overall health of our population. Science has made great strides, medical practices and procedures have made great leaps forward and even our medication breakthroughs have been astounding. Yet, today people are not taking advantage of the Health Services Industry offerings in a timely and preventative manor. As with all complex and society wide issues there are many areas to analyze and review. The core focus of this review will be on ways health services, with a focus on Hospitals and Community Health can create an environment that is focused on building patient/people environment experiences to break down the barriers of fear to seek medical attention and advice. We also examine how technology can be leveraged to enhance patient engagement and experience as they navigate the healthcare continuum. Some of the reviewed technologies are analogous between hospitality and healthcare and others are specifically focused on areas of future healthcare innovation where the required technologies are still evolving.
In this paper, we will have three authors who strategically look at each industry and believe there are opportunities to bring expertise across the boundaries between healthcare and hospitality. Previous articles and studies in the Hospitality Bridging Health (H2H) space have demonstrated that there is much to learn from both professions. It is important to note here that both industries are experiencing major turmoil from COVID-19 both during the health crisis as well as emerging from the pandemic. It is hoped that the information presented will be embraced by leaders in both industry segments as well as regulators and policy makers. This opportunity to reinvent the norms may be a once in a lifetime as our old models are crumbling and new models are being created.
H2H Leadership – A Call to Action
Hopefully Health Care leaders in the multiple disciplines understand the need to transform the historical approach to health service implementation. To patients, customers, and the communities in general. As this paper explores multiple points of potential patient interfaces with the Health Services providers, it is only under the guidance of Leaders will transformation make any progress. For this to happen, it will take a bold vision and strong sustainable commitment to evolve from current practices. That is exactly where Leaders of various service providers need to step up and make a commitment to modify current practices. First a vision and then framing a new approach to processes and procedures. This will change the culture of an organization with an enhanced focus on the patient as a person/customer. This new culture will retain all the important elements to support a great health care system but include Hospitality cultural underpinnings to enhance the patient interface.
These leaders will bring the patient experience forward to reduce fears and anxieties, creating a dialogue that will encourage each to focus on a higher level of an overall healthy well-being. These leaders will open the pathways and create the vision and allocate resources for every department to make significant advances in an enhanced patient experience. Leaders will be at the start of it all guiding the transformation.
The following excerpt from two prominent Leadership authors set the concept in motion. Thanks to James Kouzes and Barry Possner for this excerpt from their Leadership Development Institute and their books on The Leadership Challenge.
Places We Have Never Been Before
Beyond the horizon of time is a changed world. A world different from today’s world.
Some people see across this boundary of experience and into the future. They believe that dreams can become reality. They open our eyes and lift our spirits. They build our trust and strengthen our relationships. They stand firm against the winds of resistance and give us courage to continue the quest.
We call them leaders. They take us to places we have never been before. We are fortunate that they do.
Leadership says the author and sociologist Vance Packard, Appears to be the art of getting others to want to do something that you are convinced should be done. The questions for leaders, then, are How do I get other people to want to follow me? How do I create an open climate in which people want to move forward together with common purpose?
To find the answers, we asked over 500 managers and executives to describe their “personal best” leadership experiences. Their responses revealed a consistent leadership strategy and common set of practices leaders use to get extraordinary things done.
The three words that best describe this leadership strategy are VISION, INVOLVEMENT, and PERSISTENCE. To implement this strategy, a leader challenges the process, inspires a shared vision, enables others to act, models the way and encourages the heart.
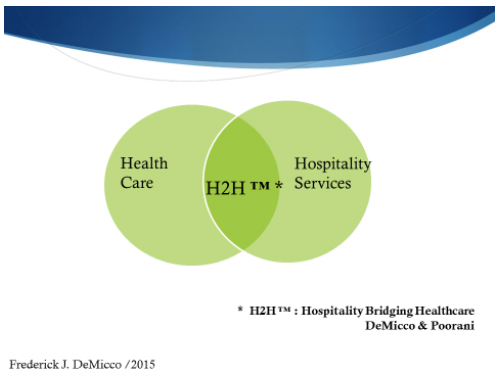
Introduction to Hospitality Bridging Healthcare (H2H) and the Systems Model Applied to Healthcare: The Role of Technology
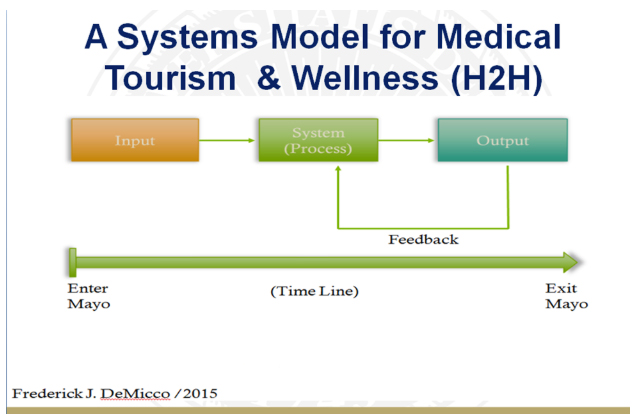
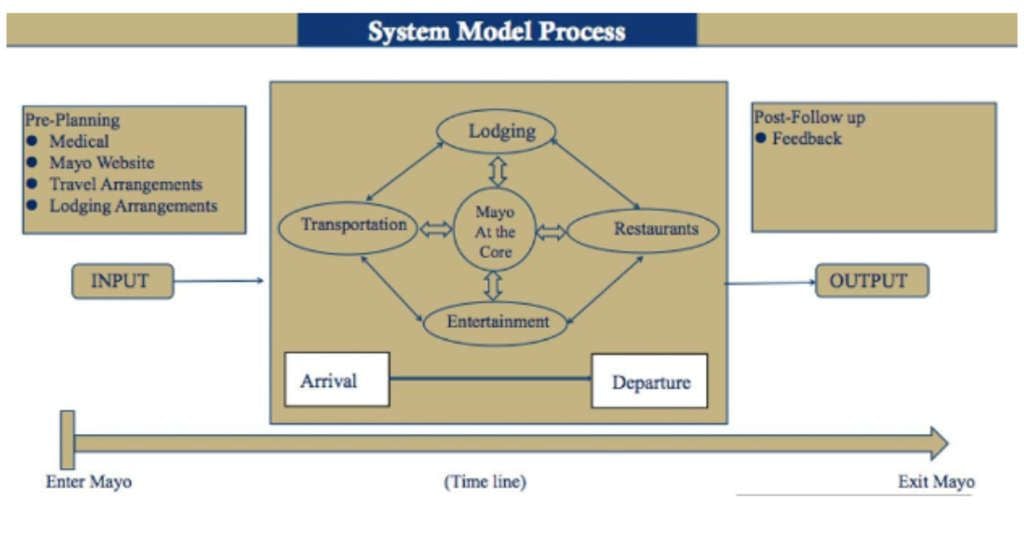
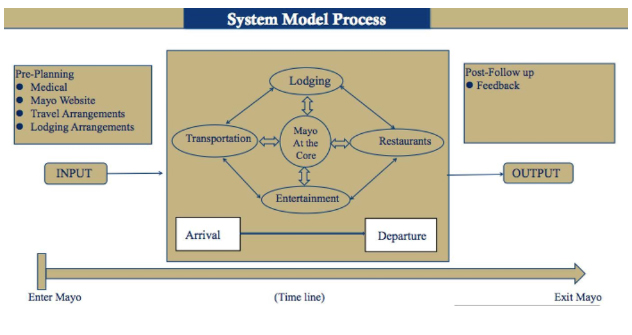
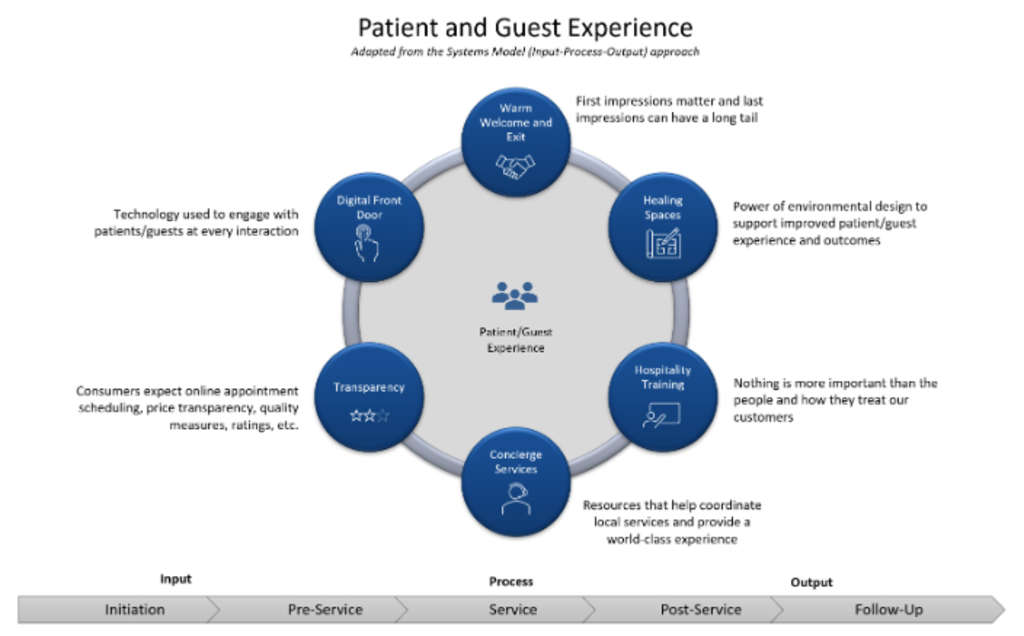
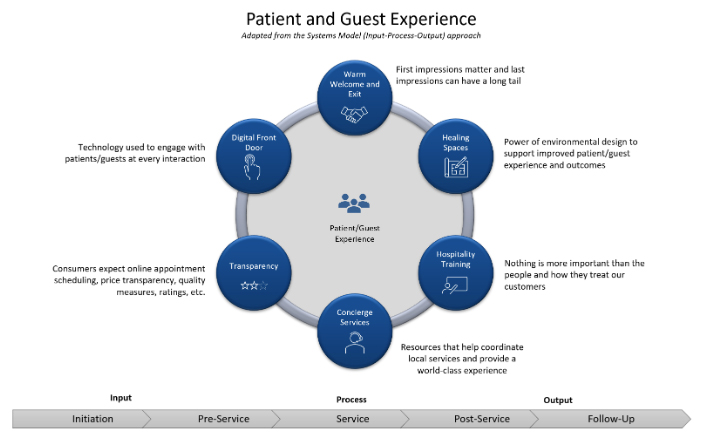
A systems model approach used in manufacturing and services can be applied to the medical and healthcare integrated with the Hospitality Bridging Health (H2H) model described below. A system comprises multiple views such as planning, analysis, design, implementation, deployment, structure, behavior, input data, and output data view. A system model is useful to describe and represent all these multiple views. The Figure below describes the Systems Model (DeMicco, F.J (2017).
The Systems Model presented above provides a vantage point for desirable patient/ guest services and outcomes. The Mayo Clinic Systems Model (as an example) provides a roadmap or blueprint for the integration of all of the services from the Pre-Mayo (before entering into the H2H System) to the Post-Mayo (The exiting from the Healthcare System) and the many of the Patient/Guest processes in between. The understanding of this model can lead to a positive level of Patient/Guest satisfaction which can lead to loyalty and positive health outcomes.
Patients travel to seek out high quality and affordable medical services all around the world. This can necessitate the patient/guest staying in a hotel. The two H2H entities should mesh and work well together for an optimal Patient/Guest services experience (DeMicco, F.J (2017).
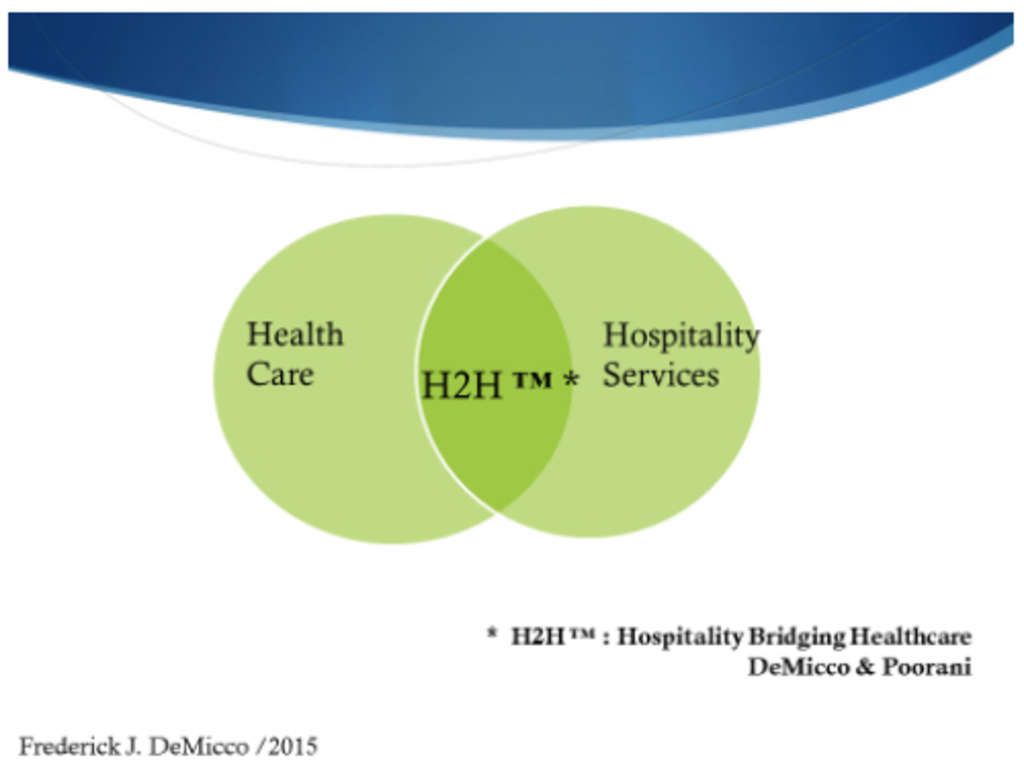
In Hospitality Bridging Healthcare or H2H (DeMicco, F.J (2017), the hospitality to healthcare (H2H) focus should align and complement each other. In fact, about seventy-five of the Patient/Guest health deliverables are actually “hospitality” related services. The careful integration of the H2H system model theme will help to achieve an optimal level of service and bring about a positive medical Patient/Guest experience. These relationships are demonstrated in the Figures below.
Applying the Systems Model to H2H
The Figure below presents a flowchart of the Medical Tourism process from input stage to output. For example, under “Pre-Mayo” systems model, Patient/Guests make initial plans to travel to Rochester, Minnesota, do their trip planning, schedule appointments, and other procedures in the process. In examining the trip planning or Input stage, the myths or uncovered misinformation included the Patient/Guest visitors are well aware of various transportation and travel options, including the Mayo Concierge service, travel services, etc. (DeMicco, F.J (2017). This was not the case.
The reality is, visitors, e.g. the Patient/Guests are likely uniformed as gathered from Mayo Clinic guest comments. There is thus a need for trusted, visible sources of information to show the range of medical travel-related services that the Mayo Clinic offers. In looking at guest perceptions of the actual travel to Mayo many guests do not know what the best means is. Should they drive since they may need a car to get around to their appointments? One couple drove from Delaware for this reason; only to find out they could have flown, since the hotels provide shuttle services to the clinics for their appointments. Therefore, better information is needed to assist medical visitors, so they fully understand the range of transportation options available to them. Regarding the booking of hotels at Mayo Clinic Patient/Guest are concerned with the price and location of the hotel rooms, but also care about comfort and amenities once they are in Rochester. They often regret their choices of lodging and try to switch their rooms. Therefore, on the Pre-Mayo planning Input side of the H2H Systems Model, better information is needed to help Patient/Guests consider the menu of lodging rooms available and the amenities that are important when making their initial reservation (Figure below) (DeMicco, F.J (2017).
The following discusses the Patient/Guest processes once inside the Mayo System (model). This includes transportation to and from Rochester, Minnesota, the hotel lodging, dining, and entertainment perceptions while in the Mayo system. Transportation within Rochester is also of concern. The reality is the public transportation is good, and the hotel shuttle system is effective and efficient. But trusted and up to date information on transportation to and from lodging to dining, lodging, and the entertainment to encourage use and exploration is required. (An App can be designed for smart phones and/or better signage, or up to date website). (DeMicco, F.J (2017).
The dining experience is another area that needs attention once in the system at Mayo. The myth is that food is solely for calorie replenishment. However, Patient/Guests and their families view meals as providing more than just nourishment, as dining out offers an opportunity to connect with someone else (DeMicco, F.J (2017).
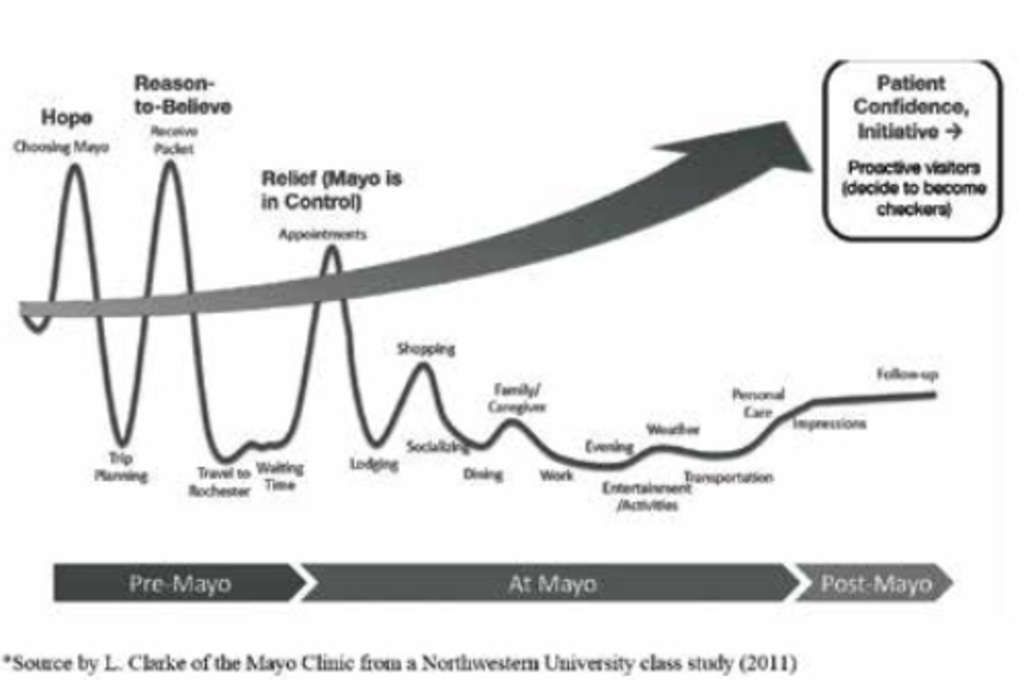
THE MEDICAL TOURISM ANALYSIS MAP (MTAM)
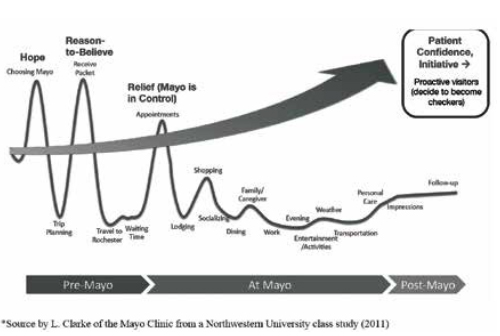
The emotional journey of the visitor within the Mayo System is mapped in the Figure below. Presented are the Systems Model stages from Pre-Mayo to the Post-Mayo or the Output as identified in the Systems Model is shown. It is possible to thus see the highs and the lows of the Patient/Guest experience, as they can offer solutions for improvements.
It should be noted that Patients/Guests most always rate their Mayo Clinic medical treatments as High, but the hospitality related services not as highly. Thus, there is an opportunity for improvement here. The Figure represents this diagrammatically below.
The Output stage of the Systems Model involves collecting feedback on Patient/Guest satisfaction through surveying both written and/or online surveys. The information collected can be used to improve the overall process for enhanced Patient/Guest satisfaction. This feedback loop is necessary to bring about continuous quality improvement in the system at Mayo and other healthcare systems (DeMicco, F.J (2017).
Industry Background
As with many industries, healthcare and hospitality are constantly faced with forces of change from all sides. Many of these forces are generated from the evolving regulatory world, market conditions, and technological innovations. Our current environment has required us to change in unprecedented ways in a relatively short amount of time. We are being pushed to adapt to a changing landscape with new rules and new opportunities. Because of these constant forces, organizations that can thrive in a changing environment have a significant competitive advantage. Think for a moment about how much has changed in the past few years from a healthcare delivery and hospitality standpoint. Entire industry segments have been dismantled to prioritize limited resources and new opportunities have been born based on the unique needs of our current environment. As organizations embrace and adapt, or elect not to embrace these changes, it will define future stability and market share.
One of the key areas that differentiate hospitality and healthcare is the culture of many hospitality organizations is father along with adoption of digital tools whereas many healthcare organizations have yet to fully embrace these technologies. Over the past few years, the foundation has been set to allow us to engage with our patients in new ways. A growing number of patients expect their interactions with healthcare to be like their interactions with travel and hospitality. Healthcare consumers have ‘liquid expectations’ and are bringing their service expectations from other industries. Digital technologies like remote patient monitoring, virtual visits, wearables, and mobile apps not only enable better care, they will also help control the costs of healthcare in the long-run. In addition, many of the digital tools that have been embraced by hospitality will help healthcare organizations create durable and enduring relationships.
An Industry’s Growth and Transformation
As we look backwards in time, the Airline Industry can serve as a great example of growth and transformation. While it is not exactly like the Health Care Industry of today, there are great examples where Leadership came together with multiple stakeholders to evolve processes and functions which today allows for an interactive and global experience. Much can be gleaned from this to apply to the future of Health Care services. The reader may want to dig deeper into the multi stages which are summarized here. Google Online Booking History and search the descriptions from AltexSoft.
Starting in the initial era of 1957 – 1976 we experienced the initial growth surge of commercial aviation. American Airlines was in a leadership role in this industry and was led by strategic plans to grow the airline and create the history of commercial airline passenger traffic. In a meeting with an IBM customer development engineer, the conversation centered around what could IBM and American do together to assist in meeting the issues of an airline. Remember this was back before transistors transformed computing power. It was the era of the punch card. The conversation over the next few years in developing early versions of SABRE (Semi-automated business research environment). This system first assisted in airline scheduling and tracking aircraft and soon evolved into early versions of selling passenger tickets, via the development of CRS (Computer Reservations Systems).
The next era cited is 1978 – 1992. The key advancement during this era created the GDS (Global Distribution System). In addition, the deregulation of the airline industry by the US Government allowed for what became unprecedented growth of airline routes as well as additional airline companies. It also allowed a global sharing of information for airlines and passengers. This too reshaped the industry and the markets along with new jet powered aircraft.
The next big phase was 1994 – 2019 which saw the creation of the internet. This expanded globally and again allowed access to companies on a worldwide basis easily and efficiently. The industry saw significant growth both in total traffic as well as expanding into smaller markets and interconnecting around the globe with both business as well as leisure travel. The growth rates were phenomenal.
The last stage to look back on is 2009 -2019. This is most noted for two significant issues. The first is the Mobil Technology applications on a worldwide basis. The second is the transition from Travel Agency ticket distribution to internet printing your own. An almost 65-year journey that will see further enhancements in the future.
A significant issue in utilizing this example is the industry of commercial airline traffic was in its infancy. Technology and applications of these new technologies were integrated into the airline industry as they were developed. The vision of Leaders adapted and adopted to these developments all with an unending strategy of creating a more consumer focused, safer experience that would remain affordable in an expanding global demand. A core principle was and is to have a focus on the individual user experience e bringing hospitality mindset into the airline service industry All stakeholders, over time, came together to integrate and develop the airline industry of today. The goal of this example is to stimulate thinking around new and
enhanced models for Health Care service providers for the future. Yes, it will be more difficult than building a new industry, but many of the developments that were implemented in the Airline industry have not been significantly included in Health Care systems of today. Hopefully, this serves as a call to action in Leadership strategy for enhancing the Health Care system of tomorrow. With various technology tools packaged with the Hospitality mindset of a positive customer experience.
Lodging Industry Journey
As we see below the Lodging and Hospitality industry has had a much longer journey with the focus of attracting customers. This is not to suggest that Health Care is focused on attracting customers but does suggest that there is a definitive need to focus on patients as a guest/customer. Over the many more years than the airline industry, hospitality is currently in a growth stage of reinventing their service offerings. As we look at lodging as another example, we can see the intersection of technology interacting in both Airlines and Lodging. Many lessons learned in earlier years have shaped the concepts of perception for today and the future. A brief look at the simplified timeline will demonstrate a progressive changing expectation by the customer/guest.
The following will focus on a few of the 40 plus key developments to bring us to what we know of the Hospitality industry today.
1809 First Hotel in the US with modern amenities, The Tremont in Boston
1894 First hotel with in-room telephones, The Netherlands Hotel in NYC
1910 Electricity in most hotels
1927 In room radios
1946 Westin introduces the first guest credit card
1947 The Roosevelt Hotel in NYC first in room TV
1947 Westin has the first guest reservation system
1950 First in room air conditioning launched in Texas
1958 Sheraton has the first 24-hour reservation system.
1976 VingCard launches first programmable key card.
1977 Micros introduces the first sales software/hardware.
1984 Spanger Miller Systems offer first SMS guest centric PMS
1986 *SABRE Corp enters and expands bookings in hotels and car rentals.
1986 Teledex introduces hotel dedicated phone systems
1994-1996 Hotels offer worldwide bookings
1995 Voice over internet protocol (VoIP) is adopted worldwide
1996 First online Travel Agencies, Expedia and Travelocity
2000 TripAdvisor is launched as a rating system for consumers
2007 The I Phone is launched moving all to a mobile ability
2008 to Present – A myriad of new services created enhancing the guest experiences.
*Denotes the beginning of cross fertilization from the Airline Industry to the Lodging Industry.
The list above continues to add new services until 2020 when the COVID pandemic changed perceptions of guest features and guest services that are important to all stakeholders. Today as we emerge from the Pandemic, the industry continues to create and develop new service offerings as guest demands evolve such as contactless check in and mobile room key and complete check out. While not all technology is welcomed by all guests, such as QR code menus, the industry is able to respond to crisis and staff shortages in a more agile approach. These lessons can certainly support the future of healthcare by bringing guest services knowledge and technology into applicable arenas.
This major change for the healthcare industry and it will need to be supported by shifts in culture and technology. A framework was developed by our research to evaluate some of these supporting areas that cross over the hospitality and healthcare industries. As previously discussed, we have adopted a Systems Model approach to evaluate the patient/guest experience as seen in the figure below.
In this model, we explore some of the patient and guest areas of focus that would help set the foundation for the needed culture shift in health care organizations to support the new models of customer engagement and care delivery.
Digital Front Door
The concept of a digital front door represents the technologies used to engage with patients/guests at every interaction from initiation to follow-up. Patients expect their interactions with healthcare to be like their interactions with Amazon. The interactions in this area also follow the Systems Model approach and have various process points that are most relevant from initiation, pre-service, service, post-service, and follow-up. For the purposes of this paper, we will focus on the areas within that are most relevant between Hospitality and Healthcare. This area includes capabilities such as provider search, appointment self-scheduling, digital check-in and registration, and virtual visits. In all these areas, transparency is fundamental to success, and we know this because of lessons learned from hospitality and other industries. Use of digital and social media, telemedicine and telehealth, remote monitoring, and related evolving technologies are also well suited for deployment in health care practices. Still, their uptake has been relatively limited to date, for such reasons as unfamiliarity, system mismatch, and absence of reimbursement. Quickening use of these tools in health and health care will require receptivity to innovation, novel partnerships, and collaborative information and experience gathering. (Kaplan, et al., 2015).
Until relatively recently, most health systems relied on an archaic approach to scheduling appointments that was typically initiated with a phone call. Some of the barriers to easily making an appointment hurt first impressions and added to the hesitation to call back to reschedule or cancel an appointment if the time that was available ended up not working out. This compounded the inefficiencies and had the net effect of increasing the rate of no-shows and ended up frustrating many consumers.
Patient Self-Scheduling
Many health systems have started to embrace patient self-scheduling but there is a wide variation in functionality from provider to provider. The cleanest way to implement this functionality in a practice or health system would be to leverage native functionality in the Electronic Health Record (EHR). Unfortunately, many of the EHR vendors that are commonly deployed lack easy-to-use native functionality. This encourages providers to rely on third-party systems to provide the needed functionality and in doing so, widens the variability in workflows, and often requires customization that can be hard to maintain particularly when it is time to upgrade. This wide variation in functionality and adoption also makes it hard to effectively research. These inconsistencies in functionality are a hallmark of technology that is still emerging and a phenomenon that is very similar to the early days of online booking in travel and hospitality. One of the key factors when searching for care online is transparency. Appointment scheduling needs to be easy to use, have price transparency, photos, and ratings.
There is no doubt that patient self-scheduling is faster and more convenient but there is currently a lack of standardization and widespread adoption. In a recent study looking at 2 million appointments booked between Jan 2019 and June 2021, between 4% and 15% of appointments were self-scheduled. Over the study period, uptake of self-scheduling increased from 4% to 15% of kept appointments. Younger, commercially insured patients were more likely to be users. Missed appointments were lower and cancelations were higher for self-scheduled patients. (Woodcock, et al., 2022). When compared to a more mature self-service industry like travel bookings the difference is remarkable. In fact, 82% of all travel bookings in 2018 were made online via a mobile app or website, without human interaction. (Statista, 2018).
In healthcare, one of the additional factors is the complexity of entry points for a given service. Many services are provided in multiple settings and specialties and for the consumer this is often incredibly confusing to navigate. These systems are unfortunately not customer-friendly more needs to be done to overcome design-related barriers, particularly for people with low health literacy. Increasing the use of enabling technology such as voice-commanded digital assistants, artificial intelligence, and natural language processing could make the systems cater to a wider range of audiences. (Dendere, et al., 2019).
Market Preference Shift to Digital Tools
In recent years it has also become apparent that there has been a preference shift from in-office appointments to telehealth appointments. Based on this research, more than half of U.S. patients 53% say the pandemic changed how they want to communicate with their doctor. Notably, nearly half 48% indicate they would switch to a different healthcare provider if their current provider did not offer telehealth appointments. In addition, an overwhelming majority of U.S. patients who received telehealth services since March 2020 84% plan to continue using telehealth appointments in the future, citing reasons such as convenience or to avoid being around people who may be sick. (Harris Poll, 2021). Additionally, Telehealth utilization has stabilized at levels 38X higher than before the pandemic. After an initial spike to more than 32 percent of office and outpatient visits occurring via telehealth in April 2020, utilization levels have largely stabilized, ranging from 13 to 17 percent across all specialties. (Bestsennyy, et al., 2021). This preference shift is here to stay and the organizations that are offering modern and efficient digital tools have a clear competitive advantage in the new marketplace.
Another area where healthcare could learn from hospitality as mentioned previously, is guest room entertainment. When traveling, it has become standard to have access to the most popular sports, news, and entertainment channels alongside of interactive guest services that allow digital concierge features, express checkout, or browse the dining menus and order room service. In many modern rooms, guests can also pick up where they left off at home by logging into their favorite streaming services (Netflix, Prime, HBOMax, Disney+, etc.) and enjoy the entertainment options they prefer. These same services are often not offered in a healthcare setting and would offer a much more comfortable patient experience. There are also fantastic opportunities to build on the guest room features above and integrate with the electronic health record. By having this integration, healthcare organizations could provide custom content around patient specific education, information about the care team, and review the next steps in the care journey. This level of information could help improve patient satisfaction, as well as provide an opportunity to store guest preferences including preferred name, favorite foods and beverages, room temperature, children’s names, and other details to help the care team provide legendary service.
Concierge Services and Hospitality Training
Healthcare settings could also benefit from concierge services. In many healthcare facilities there is no front desk or concierge to ask for help with all the things that are so hard to coordinate and navigate during a visit. This would include everything from helping to coordinate a dog walker to finding area hotels for friends and family members. The benefits of having an intentional area to provide these services are numerous, however one of the most important to consider for leadership is the resource capacity of the clinical team which is often going above and beyond to fill the gap. Organizations that are able to invest in all the latest gadgets and technology would likely benefit and see improvements in patient satisfaction if implemented thoughtfully, but nothing is more important than the people and how they treat the customer. Leaders need to invest more in hospitality training for all patient-facing employees. The current labor market in healthcare makes this even more challenging, however patient satisfaction is going in the wrong direction for some health systems and burnout and staffing issues are a big part of the equation. It will be a stretch for most organizations to invest in H2H when they are struggling to keep the doors open and staff the ICU. However, organizations that are willing to invest now will have a clear distinction and competitive advantage in the future. Happy employees = happy patients.
Another angle for future research could explore the imbalance of healthcare spending with the things that are directly attributed to wellness. Many spaces in Healthcare are designed for care and treatment, not necessarily, wellness. Evidence-based design (EBD) research has demonstrated the power of environmental design to support improved patient, family, and staff outcomes and to minimize or avoid harm in healthcare settings. While healthcare has primarily focused on fixing the body, there is a growing recognition that our healthcare system could do more by promoting overall wellness, and this requires expanding the focus to healing. (DuBose, et al., 2018). Healing spaces are one aspect that healthcare has a fair amount to learn from hospitality. This change can already be seen in many newer construction health facilities, but many large health systems are dealing with aging physical plants that are not easily adapted to the EBD guidelines.
On the horizon
Over the last few years, the foundation has been established for a truly transformative patient and provider experience. These technologies are still maturing, but in time, they will revolutionize the way healthcare is delivered. Think for a moment about the typical office visit. Once in the exam room, from a patient perspective, there is much time spent answering questions about the reason for the visit and any background information. These questions are often geared toward completing a structured note that was developed specifically for the visit type or specialty of the practice. In many exam rooms, a provider will be documenting while conducting this step in the visit process. Often, there may also be a physical examination that will also be documented in the EHR. During these encounters, a provider is simultaneously focusing on the requirements for documentation purposes as well as the patient. During the note taking process, we have essentially reduced the provider to a data entry tool to meet the established regulatory requirements while also asking them to focus on what they are trained to do from a medical standpoint. This situation is not ideal for the patient or the provider but has become the standard. The providers should be given the opportunity to focus on the patient and not be distracted with documentation. There are a few technologies that have shown potential to turn the attention of the provider back to the patient while still meeting the established data requirements.
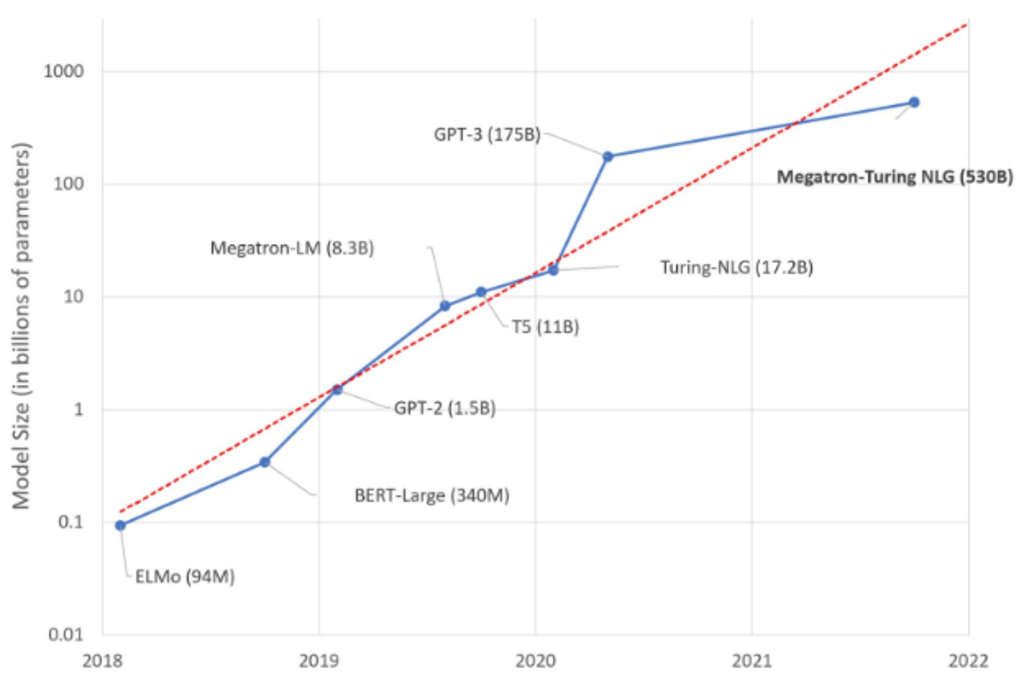
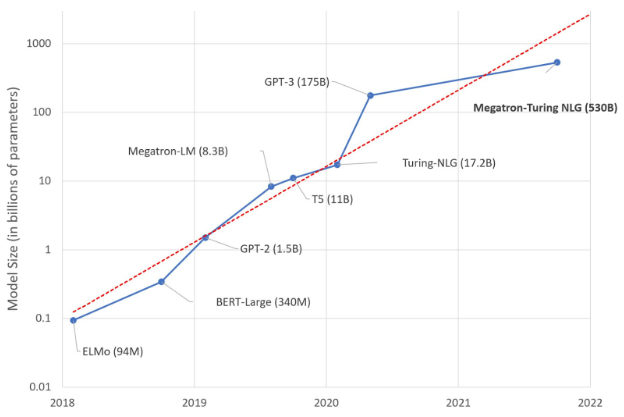
Over the past five years, there have been significant advancements in generative artificial intelligence with large language models (LLMs). Large language models are a relatively new class of model which are trained on enormous volumes of textural data. Based on the training, these models can summarize and even self-generate narratives based on inputs. One of the compelling metrics for the size of these models is to evaluate the number of parameters. Parameters are the variables that can be assembled within a model to solve based on patterns. The more parameters, the more potential sophistication in the model. Scaling up language models has been shown to predictably improve performance and sample efficiency on a wide range of downstream tasks. (Wei, et al., 2022). The figure below shows the number of parameters in some of the largest models over time.
The largest models are not, however, trained in clinical language. There is an increasing interest in developing artificial intelligence (AI) systems to process and interpret electronic health records (EHRs). Natural language processing (NLP) powered by pretrained language models is the key technology for medical AI systems utilizing clinical narratives. However, there are few clinical language models, the largest of which trained in the clinical domain is comparatively small at 110 million parameters. (Yang, et al., 2022). Interestingly, Microsoft is a majority investor in the second largest model (OpenAI GPT-3) and the co-developer of the largest model with NVIDIA.
In addition to the LLM advancements, there is another key technology that will play a role in improving the provider and patient experience. AI powered medical scribes and ambient clinical intelligence. These technologies are mainly designed to listen to a natural conversation and complete the required documentation without the need to click and type from field to field in a structured note. In early-adopter trials, these systems have shown that they can not only effectively document patient encounters, but they can also save time and reduce physician burnout. Microsoft also just acquired one of the leading technologies in this space Dragon Ambient eXperience (Nuance DAX) which may be a signal that the mega-sized generative AI models will be the next foundation to launch a highly sophisticated clinical language model that can automatically document care. This would be a significant breakthrough and has the potential to drastically improve the ability for providers to focus on the patient rather than the computer. Further study is needed to evaluate the efficiency and effectiveness of these solutions and with all the exponential growth with these technologies over the past few years, there is a critical need for more research and validation.
As these technologies mature over the next few years, there are numerous implementation opportunities in healthcare for future study.
AI Medical Summary – Leverage emerging clinical language models to summarize complex medical histories prior to beginning a visit.
AI Real-Time Surveillance – The proliferation of Medical Device Interfaces along with the volumes of interfaced data from ancillary and diagnostic studies are ideal candidates for Clinical-AI to screen in real-time to alert providers of emerging risks.
AI Clinical Decision Support – Inserting suggestions from the technology in existing clinical workflows (order entry, documentation, results review, etc.) to leverage the speed of clinical intelligence models to review vast amounts of information and empower the provider to make informed decisions.
AI Powered Coding review – Chart reviews could be conducted by the technology to help ensure accurate and complete charging and coding based on services rendered.
AI Referral Management – Based on the foundational ability of the models to predict future patterns, the technology could be leveraged to help identify the next stop on the care continuum and assist in the scheduling of future appointments based on optimizing outcomes, quality, and affordability.
Obstacles
Any new initiative will face multiple obstacles that preserve the status quo. As this paper indicates, it will take healthcare provider Leadership efforts to find ways around and through some of the major obstacles that exist. There are no easy solutions when launching a transformative effort across all service providers. At the same time, it does not mean it is impossible. As indicated it will take Leadership to open pathways to develop and negotiate new methods and processes to ensure the medical needs are met, as the people are treated in a friendly and more conducive way to seek medical treatment and advice. The following are by no means the total list of potential blockages areas but are significant areas that dominate the current observable processes and procedures experienced by customer/patients and medical support family members.
Legal Requirements
There are a tremendous number of various legal rules, statues and laws that surround Health Care. It would not be reasonable to expect this list to be reduced or eliminated. The fact is that when more and more of Health Care services are provided/paid for by Government and insurance carriers, this list will expand. These need to and must be discussed and presented in such a way that is understandable by all yet does not act as a deterrent to services needed.
There is an interesting phenomenon taking place in Health Care leadership today where this pendulum of emphasis is taking on an even bigger role than before. If you look at the current criteria of many senior executives in Health Care, they have all or part of their roots in Legal backgrounds, not Health provider experience. When you combine this along with Federal and State Policy writers, and Insurance teams, the entire system is heavily focused on Legal context and not patient services as in the past.
Insurance/Payment
This area becomes even more complex. It is typical that an individual has little to no idea what coverage they may or may not have. Even for those who have a good understanding of the insurance products, it is often overwhelming. Unfortunately, the only time a person understands what is covered is only after receiving medical services. We have called this as well as other cost issues a “price transparency” issue. Actually, it goes beyond the actual price that would be charged, as the current system in many cases does not provide financial numbers until services are committed. This lack of being able to obtain “hard” financial numbers is a significant blockage for patients. This goes back to the macro issue of understanding what benefits are received with multiple plan options. Complexity exceeds average consumer knowledge or ability to comprehend.
Status Quo
It has been stated many times that the biggest obstacle to Change is Status Quo! Marshall Goldsmith has written an entire book on this subject along with many additional authors. The status quo operation moves forward slowly and becomes the “keeper” of many forms, processes and forms. Many times, with little more regard than we are required to do this. Yet the impact on the patient/customer can readily turn into a showstopper. The status quo does not follow logic or even current needs but becomes an approach that moves it to a perpetual expanding system of dealing with people and health services.
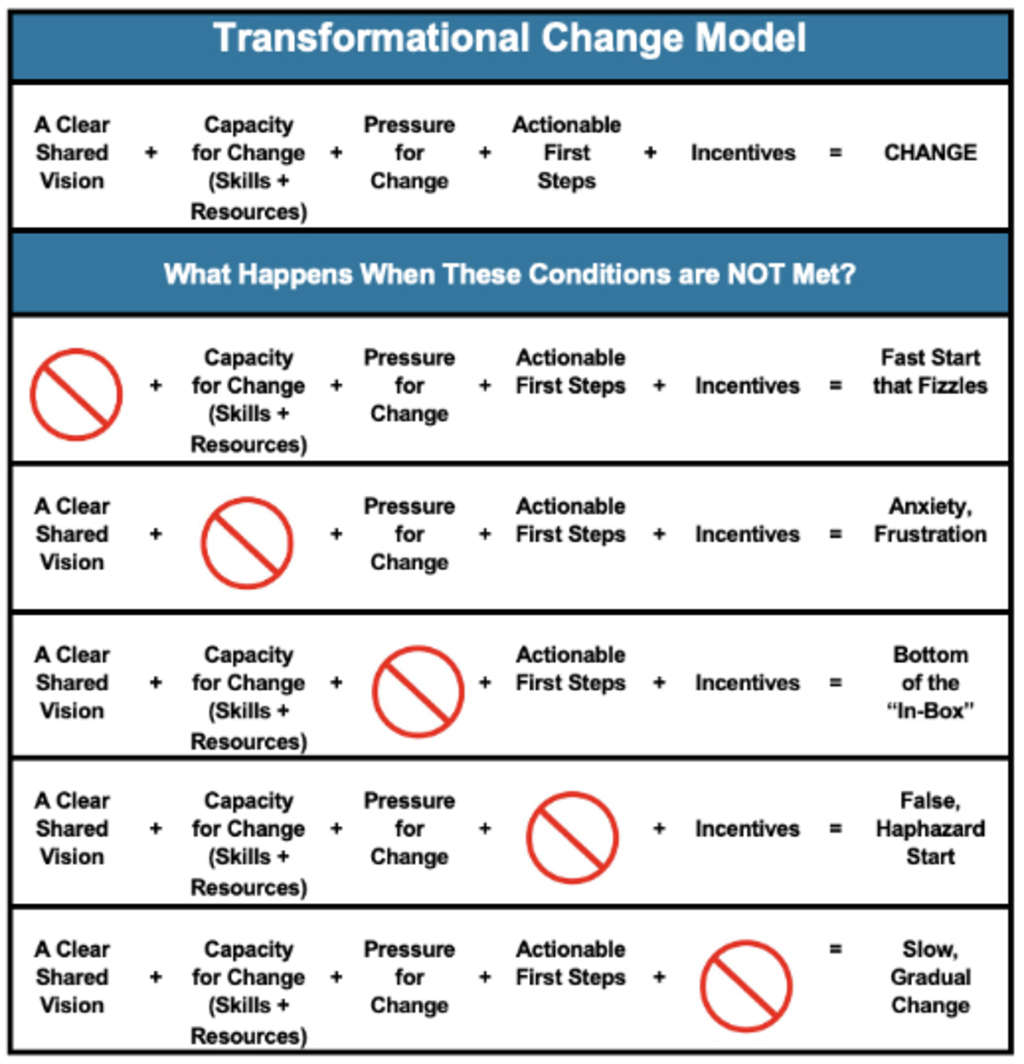
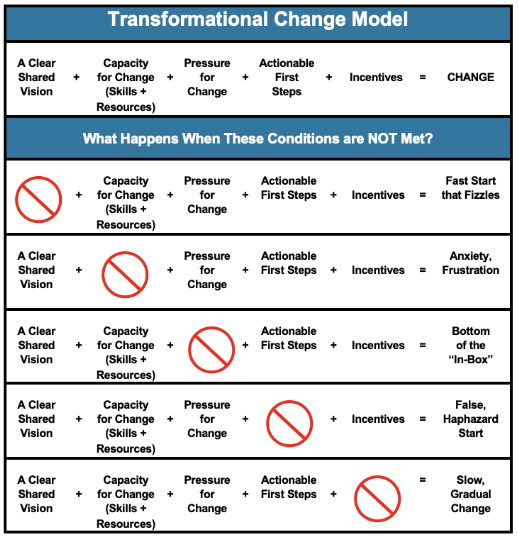
Proposed Change Template Model
There is much that will need to happen in these and other multiple areas to have any significant impact on integrating Hospitality approaches into Health Care. The following model can serve as a template for any Change Management initiatives. This was developed over twenty years ago and published by Doug Price in his book. License to Sell, 1999.
Conclusion
In summary, and as described in the Patient/Guest H2H Systems Model, at the Input stage, first impressions do matter, needs come before wants; needs are universal; wants are individual. Therefore, the healthcare facility should provide universal solutions and information about individual options, as Patient/Guests confidence in anticipation of their medical trip planning is a very important for entering into the Medical Systems Model. By understanding the steps in the process for the Patient/Guest entering into the healthcare or H2H System, and into the cascade of these processes, and eventually exiting (Output stage of the Systems Model) can help to foster a quality overall medical tourism experience. Patient/Guest satisfaction will follow, and hopefully the loyalty of the Patient/Guest will be attained (DeMicco, F.J (2017).
Information Technology at the various stages of the H2H Systems Model can help to facilitate and optimize the Patient/Guest experience.
The future of H2H and the future of healthcare have been explored to stimulate Leadership “Thinking” on a most needed transformation in the healthcare services arena. With all the pressures on healthcare reaching a new level of intensity, our goal was to provide critical thinking segments for all leaders to enhance community health and individual wellness. This in mind of how to potentially rethink process models to better serve all communities. Answers were not the objective, but critical thinking and transformative conversations are at the heart of this paper. There are no easy answers.
We have heard about many thoughts put forward by mega corporations from various industries wanting to launch into healthcare with a solution. Unfortunately, many have retreated from this market with minimal to no success. This signifies the complexity and obstacles that exist to change and transformation. But that does not mean we must live with the status quo. Collectively many segments acknowledge that change is needed both from the user as well as the provider perspective. The big lesson learned to date is it will most likely be a subsegment at a time. Examples of how other industries dealt with digital reservations are still evolving after almost 60 years of existence. This may be an entry point, but it is only one option. Where should it begin? Leaders in providers, leaders in government and public policy, leaders in insurance carriers, leaders in pharmaceuticals and suppliers, and leaders in hospitality can come together and explore positive transformation efforts. We must move forward with a concerted effort if we are truthfully focusing on delivering health services in a proactive and cost-effective approach versus the reactive approach today. A very serious but needed call to action.
It took years to evolve to where we are. Yes, we are at the best it has ever been, but we are at a plateau from the author’s perspective. We have survived the worst global pandemic we have seen in 90 years. We need to use this post-pandemic period to reach beyond what we have accomplished by thinking about new and different approaches to best serve all stakeholders. We need bold leadership to help envision “Places we have not been to yet!”
References
Bestsennyy, O., Gilbert, G., Harris, A., Rost, J. (2021). Telehealth: A quarter-trillion-dollar post-COVID-19 reality? McKinsey & Company. Telehealth: A post-COVID-19 reality? | McKinsey
DeMicco, F.J (2017). Advances in Hospitality and Tourism MEDICAL TOURISM AND WELLNESS Hospitality Bridging Healthcare (H2H). Toronto ; New Jersey : Apple Academic Press, [2017] ISBN 9781315365671
Dendere, R., Slade, C., Burton-Jones, A., Sullivan, C., Staib, A., & Janda, M. (2019). Patient Portals Facilitating Engagement With Inpatient Electronic Medical Records: A Systematic Review. Journal of medical Internet research, 21(4), e12779. https://doi.org/10.2196/12779
DuBose, J., MacAllister, L., Hadi, K., & Sakallaris, B. (2018). Exploring the Concept of Healing Spaces. HERD, 11(1), 43–56. https://doi.org/10.1177/1937586716680567
Harris Poll on behalf of NextGen Healthcare. (2021). National Survey Shows Online Access and Telehealth are Keys to Patient Loyalty. Buinesswire. National Survey Shows Online Access and Telehealth are Keys to Patient Loyalty | Business Wire
Kaplan G, Lopez MH, McGinnis JM, editors. Transforming Health Care Scheduling and Access: Getting to Now. Washington (DC): National Academies Press (US); 2015 Aug 24. Available from: https://www.ncbi.nlm.nih.gov/books/NBK316132/ doi: 10.17226/20220
Statista Mobility Market Outlook. Travel & Tourism Report – Worldwide. (2018). Statista Mobility Market Outlook. Travel & Tourism – Worldwide | Statista Market Forecast
Wei, J., Tay, Y., Bommasani, R., Raffel, C., Zoph, B., Borgeaud, S., … & Fedus, W. (2022). Emergent abilities of large language models. arXiv preprint arXiv:2206.07682.
Woodcock E, Barriers to and Facilitators of Automated Patient Self-scheduling for Health Care Organizations: Scoping Review J Med Internet Res 2022;24(1):e28323 URL: https://www.jmir.org/2022/1/e28323 DOI: 10.2196/28323
Woodcock E, Sen A, Weiner J, Automated patient self-scheduling: case study, Journal of the American Medical Informatics Association, Volume 29, Issue 9, September 2022, Pages 1637–1641, https://doi.org/10.1093/jamia/ocac087
Yang, X., Chen, A., PourNejatian, N. et al. A large language model for electronic health records. npj Digit. Med. 5, 194 (2022). https://doi.org/10.1038/s41746-022-00742-2